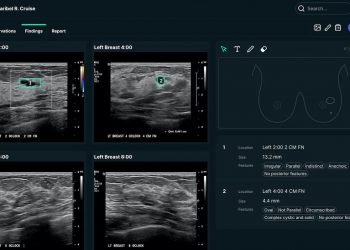
A cross-sectional study found increased EHR use among primary care physicians was associated with improvement in some quality measures, like diabetes and hypertension control and adherence to breast cancer screening.
The study, published in JAMA Network Open and conducted through Brigham and Women’s Hospital and Massachusetts General Hospital in 2021, examined 291 primary care physicians’ demographic and practice characteristics and time spent using the EHR.
PCPs spent an average of 145.9 minutes daily on the EHR in total. Significant associations were noted between EHR time and panel-level achievement of hemoglobin A1c control, hypertension control and breast cancer-screening targets.
“In adjusted analyses, each additional 15 minutes of total daily EHR time was associated with 0.58 percentage point greater panel-level hemoglobin A1c control, 0.52 percentage point greater hypertension control and 0.28 higher breast cancer screening rates,” the study’s authors wrote.
“Each daily additional 15 minutes of in-basket time was associated with 2.26 greater panel-wide hemoglobin A1c control, 1.65 percentage point greater hypertension control, and 1.26 percentage point higher breast cancer screening rates.”
Researchers noted the study has limitations, as it focuses on only two academic medical centers with PCPs and their practices may not represent the broader U.S. primary care population. Both facilities also have established population health programs that may influence ambulatory quality outcomes for the PCPs involved in the study.
Researchers also noted a lack of data regarding specific PCP-patient interactions. They were, therefore, unable to adjust for other factors, such as continuity of patient care, individual patient interactions with staff and the number of consultants involved in a patient’s care.
“Although increased EHR time is associated with burnout, it may represent a level of thoroughness or communication that enhances certain outcomes,” researchers wrote. “It may be useful for future studies to characterize payment models, workflows and technologies that enable high-quality ambulatory care delivery while minimizing EHR burden.”
WHY IT MATTERS
Although increased communication between patients and physicians via EHR may lead to improved patient outcomes, clinicians are experiencing burnout at record levels.
A survey of doctors published earlier this year shows overall physician burnout rate spiked dramatically following the emergence of COVID-19, measured at 62.8% in 2021, compared with 38.2% in 2020.
Additionally, a study published in Mayo Clinic Proceedings revealed dissatisfaction among physicians with EHR, wherein 870 physicians took part in a survey evaluating the usability of EHR. The healthcare providers rated the usability of current EHR systems, using a standardized metric, as “not acceptable” or with a grade of F, and a strong relationship was present between EHR usability and physician burnout.
Source by www.mobihealthnews.com